Managing payer enrollment in-house often stretches staff thin, delays reimbursements, and creates unnecessary stress for providers. Outsourcing this critical task not only reduces administrative burdens but also ensures faster, more accurate enrollments.
Blog
Avoid common payer enrollment mistakes that cost your practice time and money. Learn how Preferred HCP helps you streamline credentialing.
Missed credentialing deadlines drain revenue and risk compliance. Learn how Preferred HCP keeps providers active, enrolled, and paid on time.
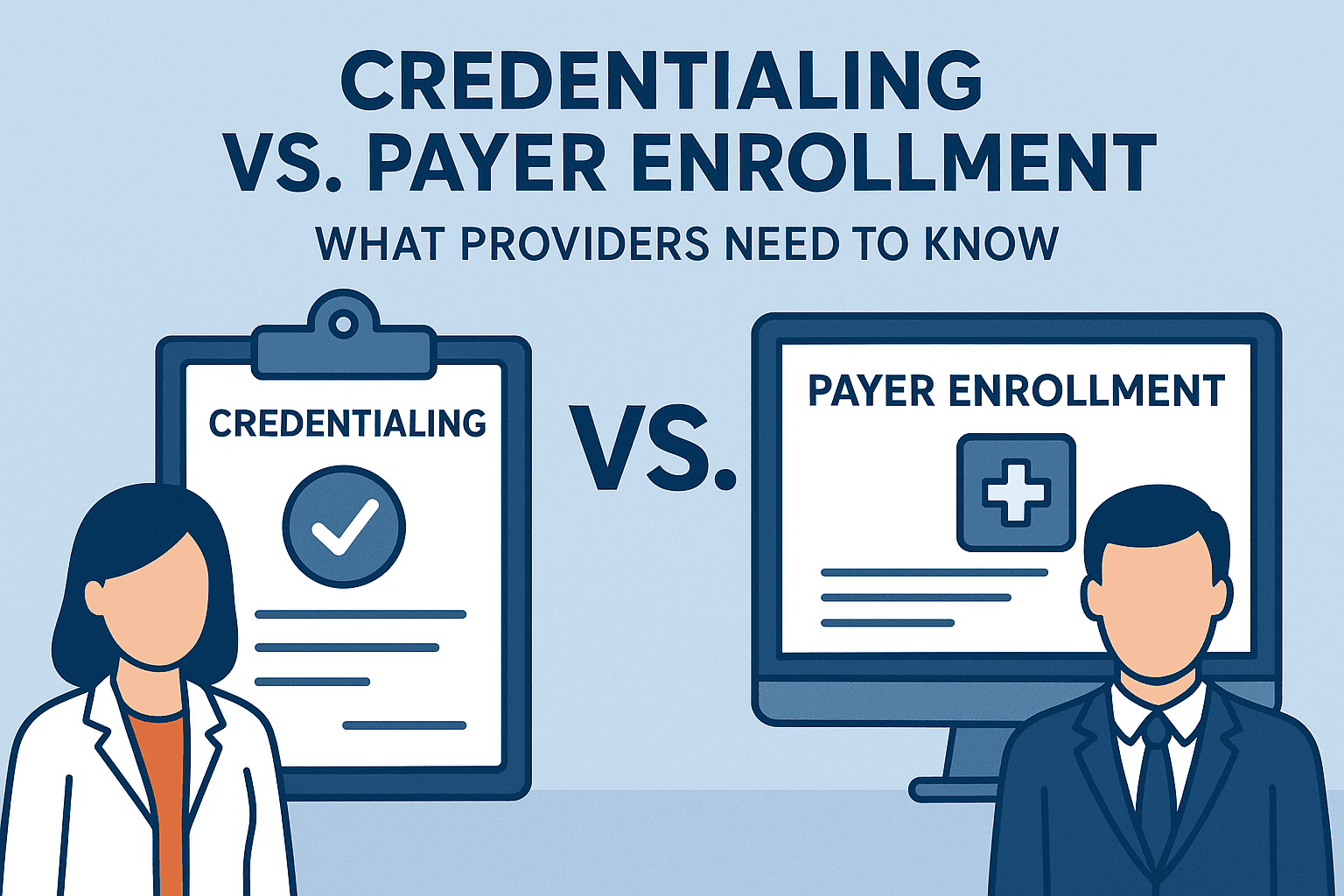
Credentialing and payer enrollment are not the same. Learn the difference and see how Preferred HCP keeps your practice compliant and revenue moving.
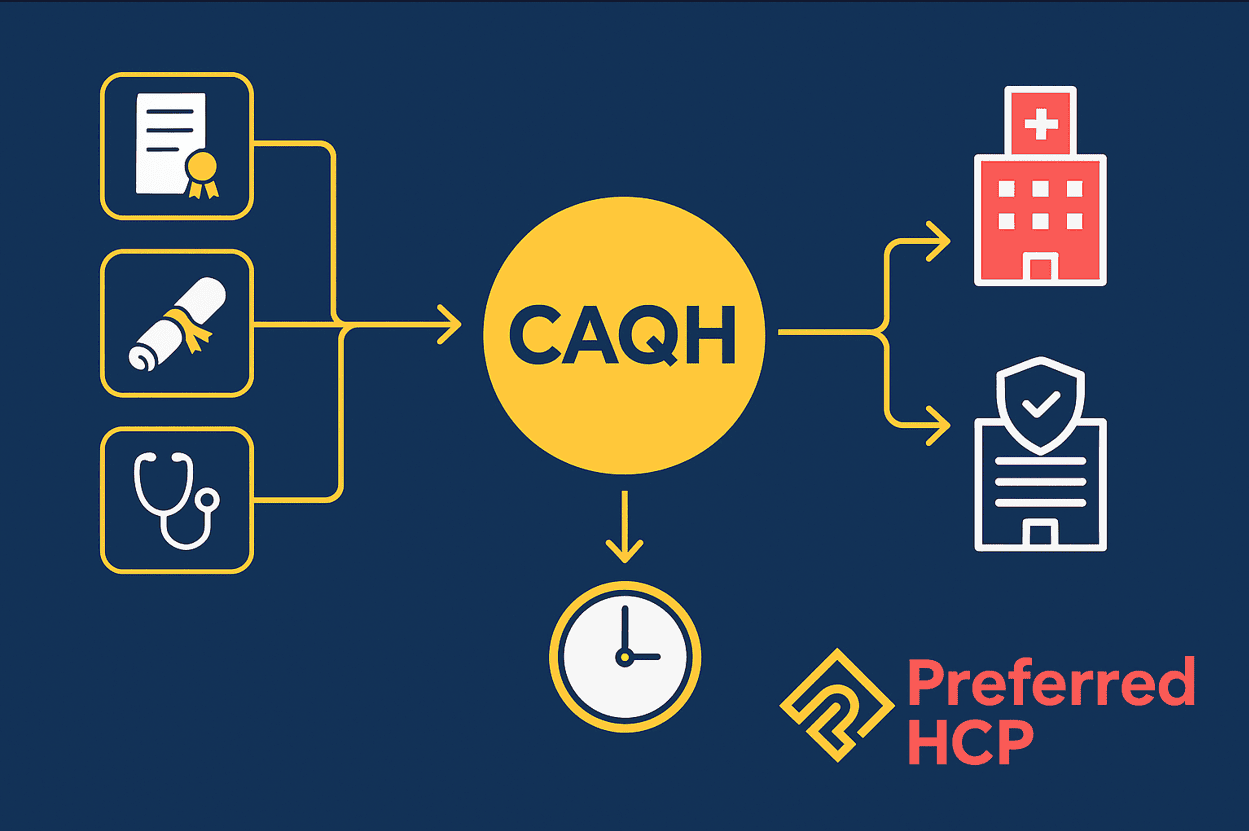
Discover CAQH: the centralized database used by 1,000+ health plans for provider credentialing. Outdated profiles or missed 120-day re-attestations cause enrollment delays, held claims, and lost revenue. Preferred HCP keeps your CAQH complete and current so you get paid faster.