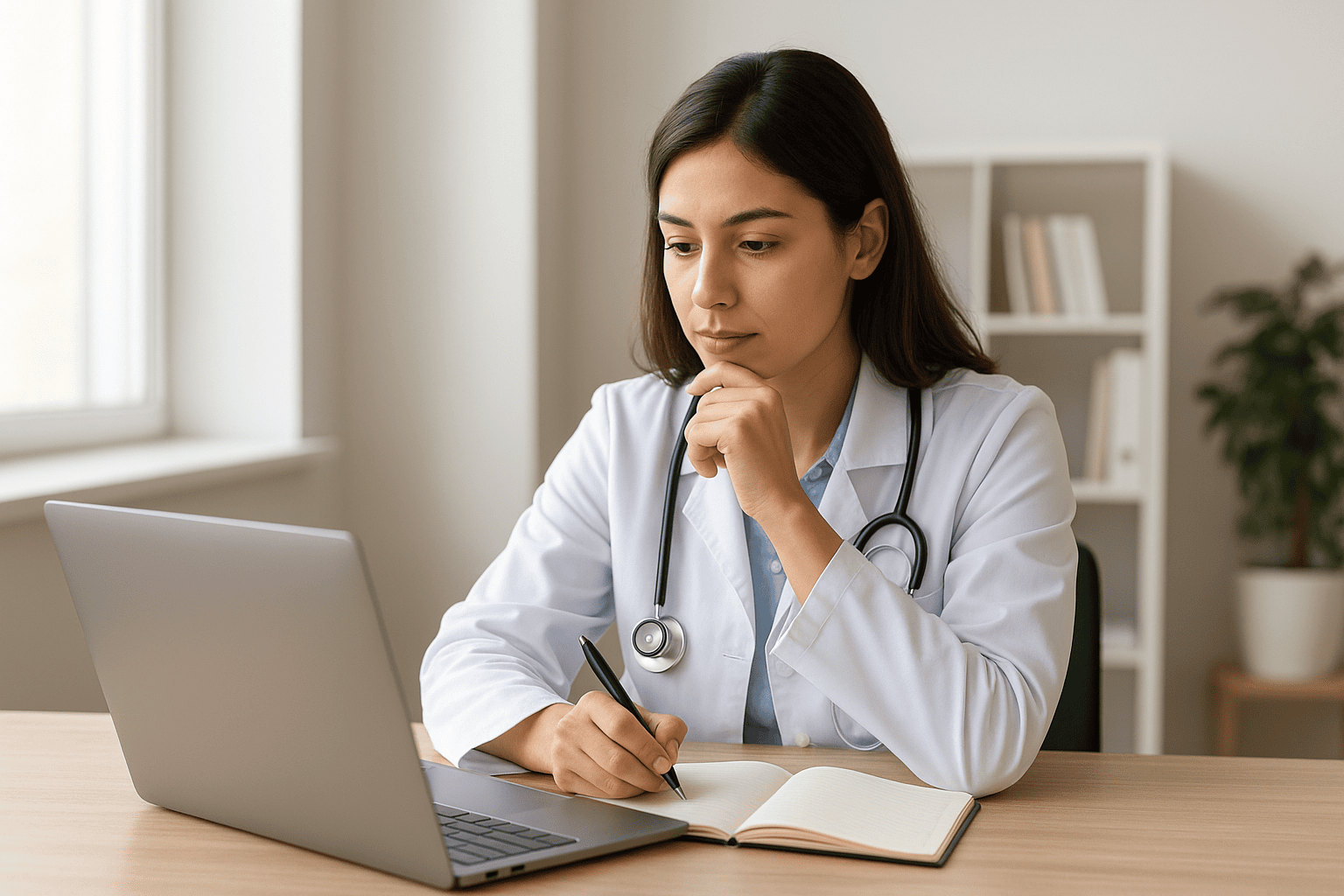
Mastering Credentialing Renewals: Track Healthcare Licenses, DEA, and Credential Expirations in 2026
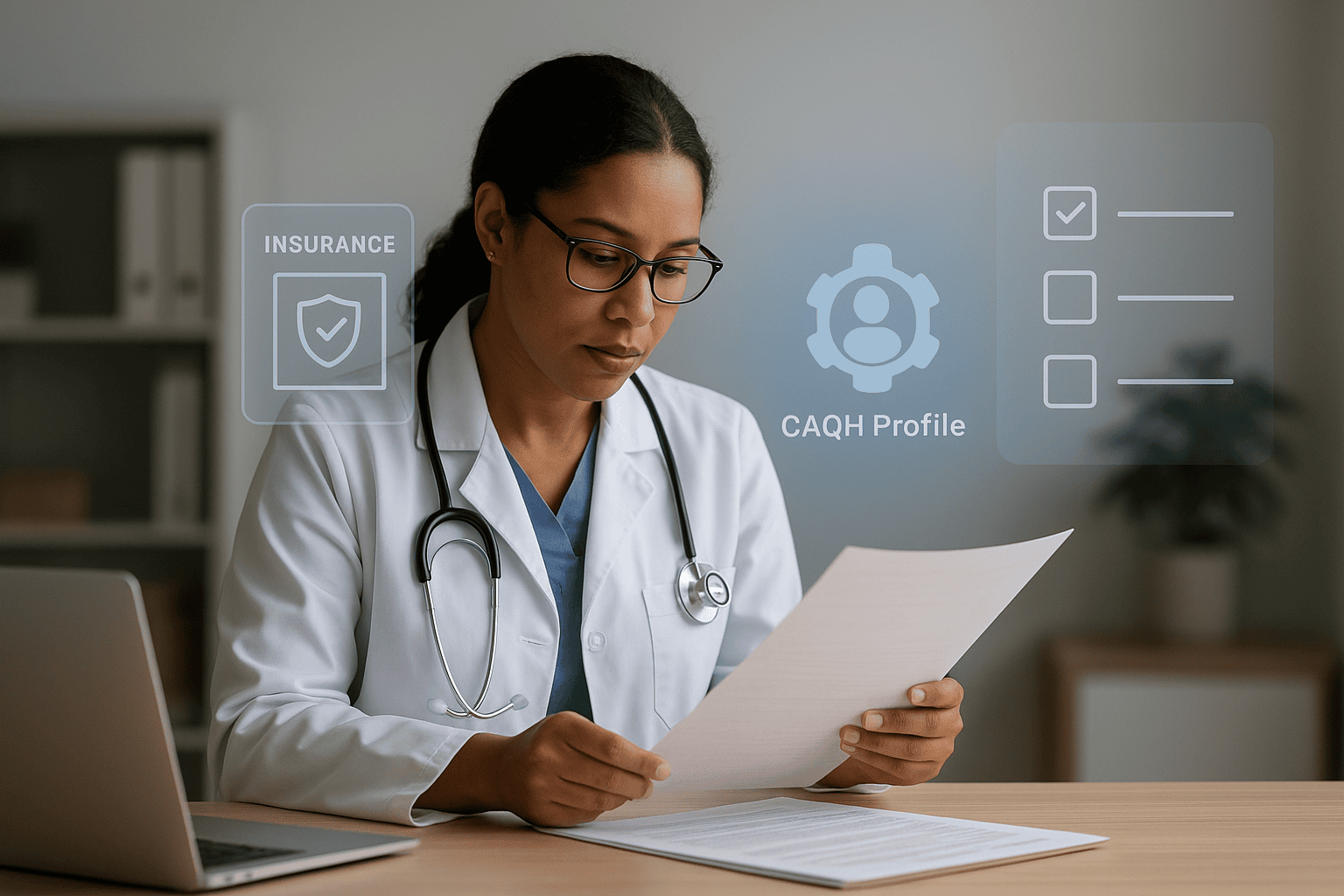
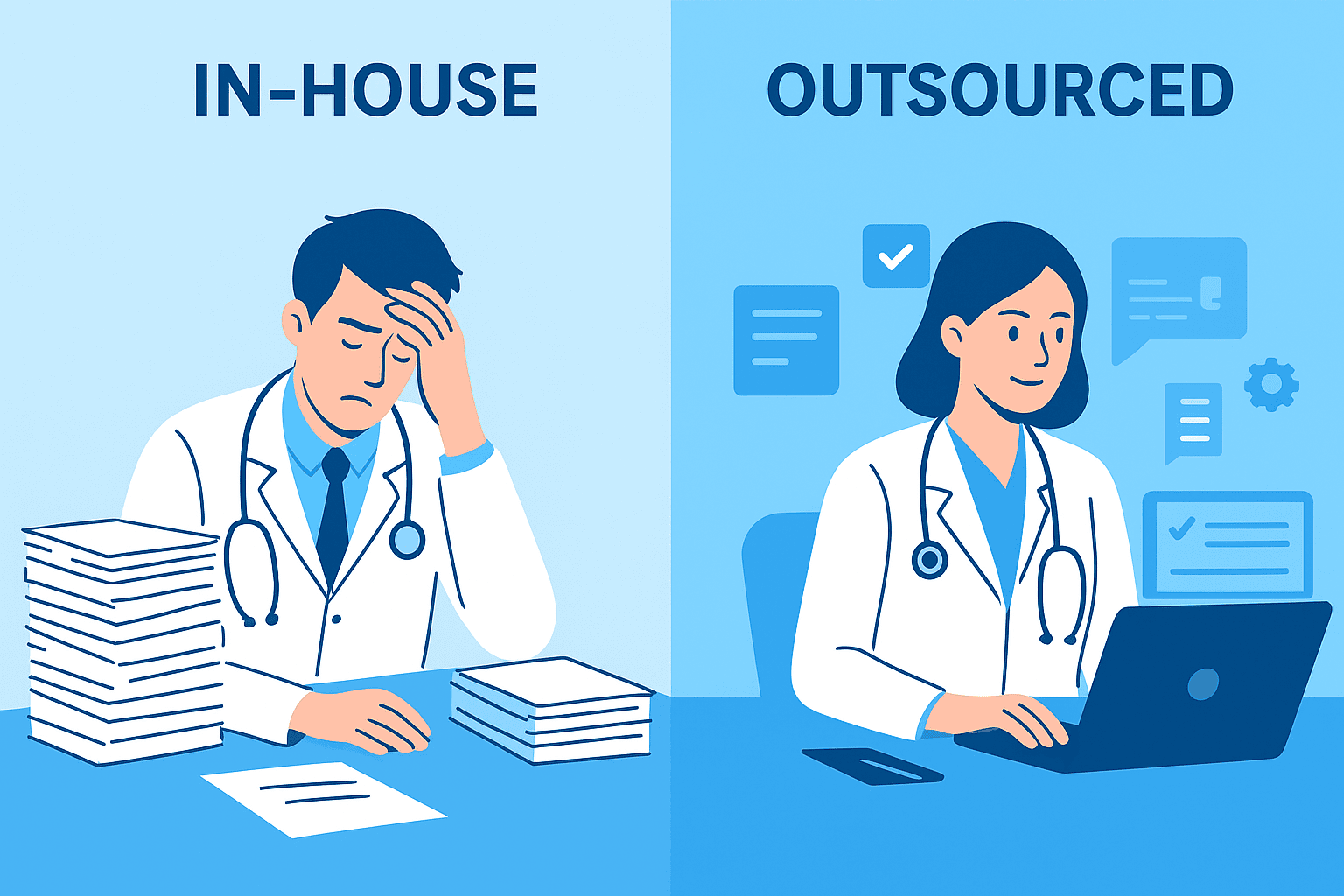
Missed credentialing renewals cost healthcare providers thousands. Learn how to track licenses, DEA registrations, and other expirables, avoid common pitfalls, and prevent costly oversights with Preferred HCP’s maintenance service.